Skin cancer was first described by the French physician, Rene Theophile Hyacinthe Laënnec (1781-1826), who is also the inventor of the stethoscope. It was an advanced melanoma with metastasis in the lung (1,2).
Skin cancer is one of the most common cancers worldwide. By age of 70, 20% of Americans will be diagnosed with skin cancer leading to a total treating cost of $8.1 billion per year only in the US. Skin cancer is characterized by an abnormal growth of skin cells, most often in skin exposed to the sun. There are two main categories of skin cancer namely, skin carcinoma and melanoma.
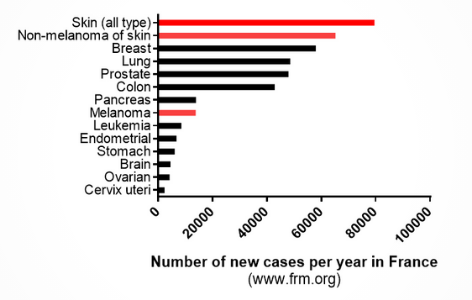
Source: frm.org
1. Skin carcinoma (Non-melanoma of skin):
By definition, skin carcinoma are tumors of epithelial origin. As the prognosis is good (survival rate higher than 95%), it is basically not known among the population even though more than 5,000 people worldwide die of this disease every month. Two main forms of skin carcinoma are differentiated as: Basal Cell Carcinoma (BCC) and Squamous Cell Carcinoma (SCC).
Basal Cell Carcinoma (BCC) is the most common form of skin cancer. It develops from the deeper layer of the epidermis because of DNA damage coming from exposure to UV radiation from sun or indoor tanning. Since BCCs grow slowly and rarely spread beyond the original tumor site, most of them are curable with minimal damage. But if they are allowed to grow and left untreated for a while, BCC can be disfiguring and dangerous. Gold standard treatment of BCC is usually surgery (named Mohs Surgery) to remove the tumors and a small margin around it.
Squamous Cell carcinoma (SCC) is the second most common form of skin cancer. Though the prognosis is very good (death rate around 1%), SCC kill twice as many as melanoma in the US. SCC develop at the expense of the epidermis, in scars, skin sores or other areas of skin injury that most often are exposed to UV radiation (sun). When found and treated early, most SCC can be cured. Once again, the gold standard is surgery. Nevertheless, if SCC is more advanced, it becomes harder to treat and more dangerous as it is capable of spreading to lymph nodes, distant tissues, and organs. In those cases, radiotherapy and immunotherapy complete the array of tools at the doctor’s disposal (9,10).
2. Melanoma:
Melanoma is the most serious form of skin cancer, it begins in cells named melanocytes which gives color to the skin and are located in the upper layer of the skin. Only 20-30% of melanoma is developed from moles and in most cases, it is developed from normal skin. Contrary to carcinoma, melanoma has a high ability to spread rapidly to other organs. If not treated in 4 months after diagnosis, a patient diagnosed with a stage I melanoma has 41% higher risk of dying from the disease in comparison with a patient treated in the first month. Melanoma appears because of DNA damage in melanocyte due to UV exposure resulting in uncontrolled cellular growth. People who produce higher level of eumelanin (naturally darker-skinned people) are more protected than others from melanoma. Based on the TNM classification (T: description of the original Tumor; N: spreading to the lymph Node; M: presence of Metastasis), melanomas are classified in 5 stages.
If melanoma is still at an early stage, the gold standard is surgery to remove the tumor and margins that are bigger than for carcinomas as the melanomas are more invasive. For more advanced stage, there is more and more therapeutic options like immunotherapy, targeted therapy, chemotherapy, and radiation (9,10).
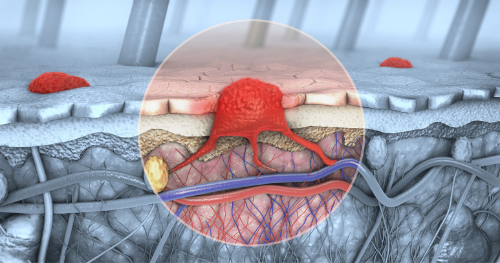
3d illustration of a cross-section of skin with melanoma that enters the bloodstream, lymphatic tract (Source: Science Photo Library)
Research on skin cancer
Thanks to research and different therapeutic strategies, survival rate of patient with advanced skin cancer, especially advanced melanoma has increased in the last 40 years. At present, 5-year survival rate of advanced melanoma with metastasis is below 50% and hence research is still very necessary to help these patients. One of the many research interests in cancer treatment recently is abscopal effect.
The abscopal effect is mediated by a systemic anti-tumor immune response and reflects the regression of non-treated metastatic lesions at a distance from the primary site of treatment. So far the mechanism is not completely understood and is difficult to predict in humans, but many research teams are work on it. In the lab, it had been observed that when immunotherapy is combined with radiotherapy or photothermal therapy (PTT) 3-7, in the latter case, PTT permits to warm the tumor leading to an increase in infiltration of immune cells (macrophage, T cells, etc.) inside the primary tumor (8). This will lead to a better recognition of malignant cells by the immune system. Combining with immunotherapy ( like anti-PD16, anti-PDL14, CAR T Cells 7) or an immunostimulant (CpG adjuvant5), boosts the immune system which destroys the recognized malignant cells.
